Dental Claim Attachments: Definition, Types, & Proper Submittal


“Oh no! My dental claim didn’t pay again!” This is often said in dental offices nationwide. But why? The truth is some claims need supporting documentation to show “proof” that the procedures performed for the patient were actually warranted.
Maybe you have someone new to your dental team that needs to know how to send claims with attachments properly. Or maybe, you just need to know which attachments need to be sent with which procedures. Regardless, if you want to be paid by insurance companies, you need to know how to send dental claims with the appropriate attachments.
Every dental office has a process for checking a patient in, completing the patient’s dental work, then walking the patient out. The patient then leaves your dental practice trusting you’ve “got it” from here, and the crown or root canal service the patient received will be paid by their dental plan.
But what if you don’t quite know what to do next with their claim?
One option is leveraging outsourced dental billing companies like Dental Claim Support. With years of claim submission experience, we know which procedures need claim attachments in order for insurance companies to process them upon initial submission.
After reading this article, you will know exactly what the next steps are. Especially, when it comes to proper dental claim attachments and getting your claims paid on the first submission.
What is a dental claim attachment?

A dental claim attachment is supporting documentation that proves the necessity of the procedure being performed. Simply put, it aids in proving medical or dental necessity.
Procedures requiring attachments should be included with the initial claim submission utilizing an electronic clearinghouse. Depending on the procedures listed, the number and type of attachments may vary.
However, it is best to submit all supporting documentation upon initial submission to prevent any delay in processing the claim. Delayed claims lead to headaches and lost revenue. Send everything you have the first time!
Types of dental claim attachments
- Narrative: written documentation summarizing the clinical necessity of the treatment performed based on the provider’s professional findings (diagnosis) of the patient’s existing condition.
- Preoperative radiograph (x-ray): an x-ray of the tooth/teeth/area taken prior to treatment being completed. This is vital for showing the existing condition of the area necessitating treatment i.e., recurrent decay, missing teeth, impacted teeth, faulty restorations, large fractures.
- Postoperative radiograph: an x-ray of the tooth/area taken after the treatment has been completed. This provides clinical evidence that the treatment was completed i.e. completion of root canal therapy (RCT).
-
- When selecting x-ray attachments, it is important to select radiographs of diagnostic quality. Meaning, they are clear and easy to “read”.
-
- Intra-oral photo/caption (IOP/IOC): high-quality photographs taken of the tooth/teeth area being treated using a small handheld, pen-shaped camera inside the mouth. This is vital for showing detail that is not captured radiographically i.e., small fractures/craze lines in teeth, the extent of decay/recession, lesions.
-
- Intra-oral photos should be void of saliva bubbles and clearly support the treatment completed. The sharper the image, the clearer the diagnosis.
-
- Additional Supporting Documentation: Periodontal charting, sedation records, sleep studies, referral reports, etc.
The more qualifying documents submitted, the greater likelihood a claim is approved and processed with the initial submission.
How do I know if my dental claim needs an attachment?
There is a loose guideline for claim attachments that most dental practices follow. However, specifications for qualifying CDT procedure codes that require attachments is plan specific.
The guideline is as follows:
For most dental plans, an attachment is not required for preventative and diagnostic services. Preventative and diagnostic services being your exams, cleanings, radiographs (x-rays), fluoride treatments, etc.
Attachments are typically not needed for a majority of basic dental services too. However, basic services such as periodontal procedures, root canals, extractions, and anterior composites may require pre and post-operative radiographs.
The reason being, insurance companies want to make sure
- The procedure was actually completed
- The procedure was necessary and not purely cosmetic in nature.
Major services such as crowns, bridges, dentures, etc. will likely always require attachments to some degree. The chart provided below sums this up nicely.
| Service Type | Common Procedures | Attachments Needed? |
|---|---|---|
| Preventive | Exams, Cleanings, Radiographs, Fluoride | No |
| Basic | Composites, root canals, extractions, periodontal services | Maybe |
| Major | Crowns, build ups, bridges, implants, dentures, partials | Yes |
Again, all of these are subject to the patient’s dental plan guidelines and can be verified during the insurance verification process.
How do I submit a dental claim attachment?
The preferred method for submitting a dental claim attachment is to utilize an electronic clearinghouse with attachment capabilities. An analogy would be an email with a picture attachment.
An electronic clearinghouse works similarly when sending attachments with claims. Depending on your dental practice management software, the exact steps to adding an attachment will vary, however the attachment itself will not.
The most popular attachment software is National Electronic Attachment (NEA) FastAttach. NEA FastAttach creates an electronic file number associated with your attachment.
Think of it like a receipt you get when you go to the post office to mail a package or certified letter. If an insurance company claims to have not received your attachment(s), you can give them that NEA number, and they can search the national database for that specific image and find your “package”.
This cuts back on all the back-and-forth between an insurance company and your dental practice. There are other great clearinghouses with similar capabilities and attachment software embedded. Also, NEA is widely known and utilized, however there are other clearinghouses with comparable capabilities.
Can I mail my dental claim attachments?
Yes, you can most certainly mail your claims with the appropriate attachments, however, there are more issues that arise when you submit your claim in this fashion.
For one, when mailing printed radiographic images, they must be printed on high-quality photo paper using a high-quality photo printer. The reason is that once received by the insurance payer, hard copy images are scanned into their system. When this happens, the quality is often compromised.
This will not give the dental consultant, the dentist reviewing the claim for benefit approval, the ability to fairly approve the treatment rendered and can possibly lead to claim denial.
Secondly, paper claims with attachments can create a tracking issue and easily become lost in transit. Without proof of electronic claim submission or an NEA attachment number, it is often difficult to dispute claims that are denied due to timely filing or those that are “lost” in the mail.
You’d be surprised how often an attachment magically gets unstapled from a claim form when it is mailed in. Delaying payment is beneficial to the insurance company and not so much for the dental practice.
How do I let the insurance company know I have included a dental claim attachment?
It is important to enter all information applicable to the services rendered in Box 35 and Boxes 38-47 of the 2019 ADA dental claim form. Submitting all pertinent information reduces the likelihood of the insurance payer requesting additional information required to process the claim, which helps you get claims approved faster.
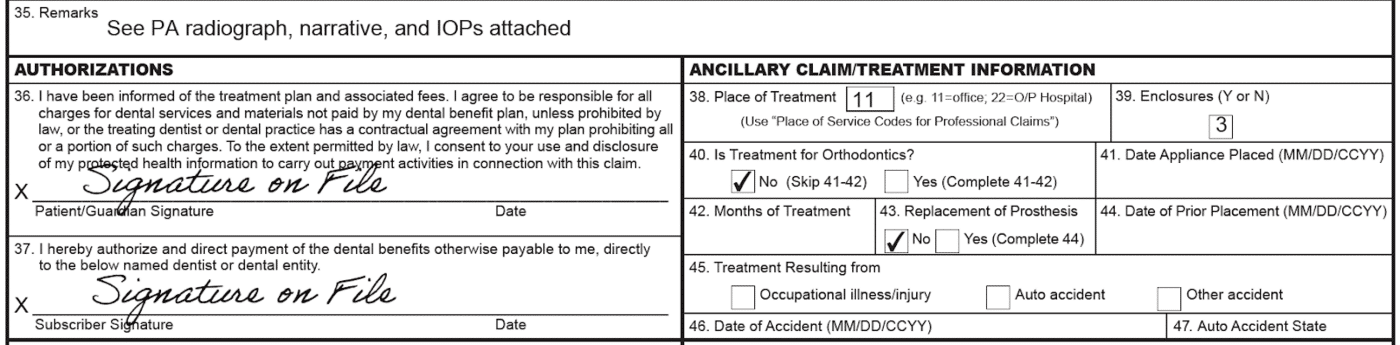 Whether you mail the claim or submit the claim electronically, the appropriate boxes need to be completed. This signifies to the insurance company that something is attached and the claim can not be automatically processed. If you do not have these boxes completed, it allows the insurance company to state they did not receive the attachment. This will delay the payment because you’ll need to resubmit the claim with the appropriate attachment(s).
Whether you mail the claim or submit the claim electronically, the appropriate boxes need to be completed. This signifies to the insurance company that something is attached and the claim can not be automatically processed. If you do not have these boxes completed, it allows the insurance company to state they did not receive the attachment. This will delay the payment because you’ll need to resubmit the claim with the appropriate attachment(s).
Dominate your dental claim submission process
This article has highlighted the importance of dental claim attachments and getting claims paid. Attachments are just the “tip of the iceberg” with claims submission though.
Cliches aside, now that you are comfortable with claim attachments, take your knowledge to the next level with dental claim submission.
Understanding the whole process for dental claim submission will not only save your dental practice money, but it will save your dental team time. To learn more about what attachments are needed for different dental insurance claims, enroll in our educational platform, Dental Claims Academy. You can take courses, participate in discussions and even earn CE credits. 
Related Posts
Dental revenue resources from Dental Claim Support
